Abstract
Background: Indolent B-cell lymphoma (iBCL) are clinically heterogeneous and accounts for 10-15% of all kind of subtypes in NHL in China. Although iBCL have a relatively good survival, majority of these lymphomas is considered incurable. The favorable activity and safety profile of rituximab monotherapy in the initial treatment of iBCL has been proven. Interferon alpha (IFN-α) has been proven to be effective in modulating immune responses and may enhance the clinical responses to rituximab in vitro and in vivo studies. Clinical combination of rituximab and IFN-α was associated with fewer early treatment failures compared to single agent rituximab. Peginterferon-α-2(peg-IFN-α2) has a longer half-life with less toxicity. It also is one of the options for the treatment of chronic hepatitis B virus (CHB) infection. Therefore, we hypothesized that peg-IFN-α2 may synergize with rituximab and would minimize or eliminate minimal residual disease (MRD). The purpose of this study is to evaluate the efficacy and safety for this combination in pts(pts) with treatment-naive iBCL.
Methods: This trial enrolled eligible pts aged 18-80 years with newly diagnosed iBCL including FL(grade 1-2,3a) and MZL. Pts were eligible if they had ECOG ≤ 2, adequate organ function and bone marrow function, and at least one measurable or evaluable lesion. Further eligibility criteria were HBsAg positivity with HBV DNA load <3000 IU/mL prior to study; serum ALT level of <5 times the upper limit of normal. During induction phase, pts received rituximab biosimilar (Henliritux ® Shanghai Henlius Biotech) 375 mg/m 2 intravenous infusion on d1. Peg-IFN-α2b (Pegberon ®, Xiamen Amoytop Biotech) was given at a dose of 135ug, subcutaneously, on d1,8. The combination repeated every 21 days for 6 cycles. Responded pts receive rituximab (every 2 months) plus peg-IFN-α2b (every month) maintenance at the dose described above, for up to 2 years until disease progression and intolerance. Simultaneously, CHB pts orally treated with entecavir continuously. The primary endpoint is ORR assessed by investigators per Lugano 2014 criteria. Key secondary endpoints included TTR, DOR, PFS, OS, HBV DNA load clearance, and safety. Adverse events (AEs) were summarized according to NCI CTCAE v5.0. All pts' blood samples were collected for circulating tumor DNA (ctDNA) assessment before treatment in each of cycles. ctDNA samples were analyzed by capture-based NGS targeting 475 lymphoma- and cancer- relevant genes. This trial was registered at ClinicalTrials.gov (NCT04246359).
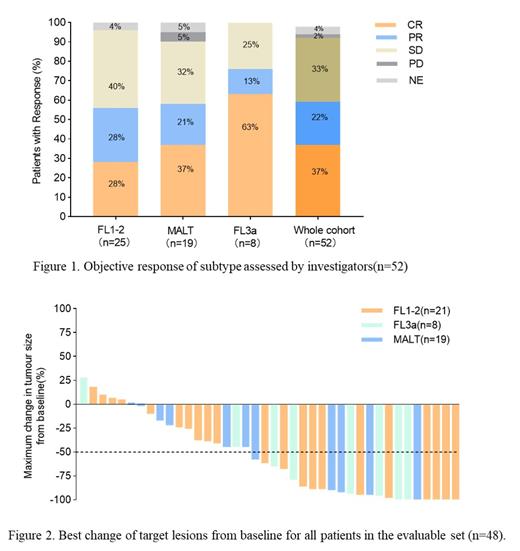
Results: From January 2020 to July 2021, 52 eligible pts with median age of 54 (range, 29-75) years were enrolled from 6 institutions in China. Thirty (54.5%) are female, 20(36.4%) pts were symptomatic and 22(40.7%) pts with FLIPI score≥3, 6(10.9%) pts suffer from hepatitis B with HBV DNA load <3000 IU/mL at study entry. At cutoff date, there were 25(46.3%) FL (grade 1-2), 19(35.2%) MALT, 8(14.8%) FL (grade 3a) pts enrolled. Of 50 response evaluable pts, 31(62.0%) pts achieved an objective response including 19(38.0%) pts with CR based on investigators. ORR were 58.3% (14/24), 75.0% (6/8), 61.1% (11/18) and the CR rates were 29.2% (7/24), 62.5% (5/8), 38.9% (7/18), 0,0 for FL (grade 1-2), FL (grade3a), MALT respectively. Median HBV DNA load clearance time was 1.8 months (1.3-2.1months), no hepatitis B virus reactivation reported. With median follow-up time was 6.2 months (range: 1.4-18.3 months), median OS, PFS and DoR was not reached; 6-month OS and PFS rate of whole cohort was 96.7±3.3%, 85.3±6.1%, respectively. Median TTR was 3.0months (1.5-5.2months). Dynamics ctDNA assay is in progress, data in detail will be reported at the ASH conference. The most common treatment-emergent adverse events (TEAEs) were hematological relevance toxicities. The most common grade hematological TEAEs (>30%) were neutropenia 63.5%, anemia 34.6%, thrombocytopenia 28.8%. Non-hematological TEAEs (>10%) were fever (28.8%), transaminase elevated (28.8%), fatigue (26.9%), infusion reaction (17.4%). Most common grade 3-4 TEAEs (>5%) were neutropenia(17.3%), anemia (7.7%). No treatment-related death occurred.
Conclusion: Rituximab biosimilar plus pegylated interferon α-2b provided favorable response in newly diagnosed advanced iBCL and was well tolerated. No hepatitis B virus reactivation was observed. Further investigation is warranted.
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal